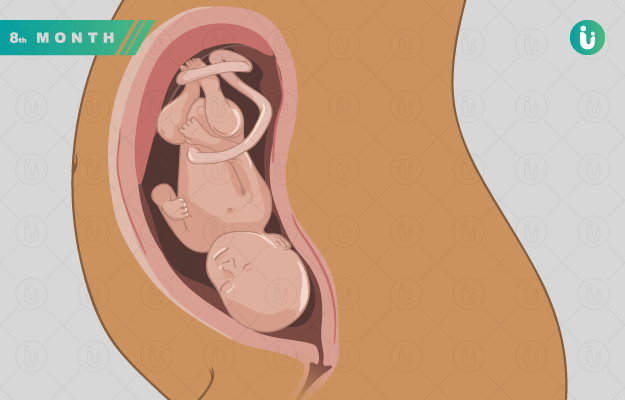
The average human pregnancy is expected to last 40 weeks from the first day of the last menstrual period (LMP) to the estimated date of delivery (EDD); however, great variations can occur, with a significant impact on the mother and baby’s health.
Present definitions describe a full-term pregnancy as lasts between the start of the 39th week and the end of the 40th week (40 weeks 6 days) and births occurring in this timeframe are associated with the best outcomes for the mother and the baby.
While early term (births occurring between the start of the 37th week and the end of the 38th week) pregnancies and preterm (births occurring anytime before the 37th week) pregnancies bring with them problems for the still-developing baby, prolonged pregnancies (those extending beyond 42 weeks of gestation) have their own set of possible complications. Around 5-10% of all pregnancies globally are prolonged beyond 42 weeks and nearly 20% of all pregnant women require induction of labour - the majority of them being post-term pregnancies.
Most often, the cause of a wrongly labelled “post-term pregnancy” is an incorrect date of the last menstrual period and wrongly-calculated estimated date of delivery (EDD). Therefore, it is essential to date all pregnancies with an early pregnancy ultrasound, preferably in the first trimester. If the gestational age of the fetus by ultrasound is less or more than three weeks of that calculated by the LMP date recounted by the mother, the LMP date is considered incorrect. The crown-rump length (CRL) and head circumference (HC), measured in the first-trimester ultrasound, are used to date the pregnancy.
The use of first-trimester ultrasounds to date the pregnancy has reduced the incidence and complications of post-term pregnancies considerably. Although the causes of prolonged pregnancy are not fully understood, some factors increase the risk of post-term pregnancies.